Complications and Side Effects of Gastric Sleeve
Though gastric sleeve is a safe procedure, it does have some complications and side effects. Compared to gastric bypass, its complication rates are lower.1
Comparison of 30-Day Mortality Rates2
|
Gastric Sleeve |
0.08% |
|
Gastric Bypass |
0.14% |
|
Gastric Banding |
0.03% |
Comparison of 30-Day Complication Rates2
|
Gastric Sleeve |
0.96% |
|
Gastric Bypass |
1.25% |
|
Gastric Banding |
0.25% |
Some of the risks and complications of gastric sleeve are discussed below:
Postoperative Bleeding
Risk reported in 1% to 6% cases3
- Blood in vomit (hematemesis)
- Black, tarry stools
- Drop in hemoglobin levels in serum (drop exceeding 10 g/L)
- Abnormally rapid heart rate (more than 120 beats per minute)
- Low blood pressure
Common sources of bleeding include:
- Sleeve staple line
- Liver
- Spleen
- Walls of the abdomen
Prevention:
A number of buttressing materials are available to reduce the risk of bleeding from staple lines. However, their effectiveness is still a subject of controversy.
Staple Line Leaks
A dreaded complication after sleeve gastrectomy in which the digestive contents seep through seal or sutures into the abdomen, staple line leak rates vary between 1% and 3% when performed as a primary procedure, and 10% when performed as a revision procedure.4
Common signs and symptoms:5
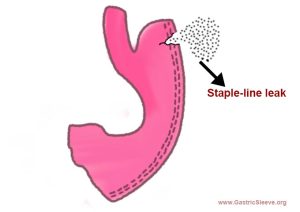 Fever
Fever- Pain in the left shoulder
- Abnormally rapid heart rate
- Quick, shallow breathing
- Changed appearance of the drain discharge
- Pain in the chest/abdomen
Prevention
- Reinforcement of staple line with extra sutures
- Intraoperative tests, such as Methylene blue dye and air leak test
- Barium swallow test
Abscesses within the Abdomen
Intrabdominal abscesses (pus-filled pockets surrounded by inflamed tissue located inside the abdominal cavity) have an occurrence rate of mere 0.7%.3
Common signs/symptoms:
- Pain in the abdomen
- Fever
- Nausea
Treatment
- Antibiotics
- Placing a drain through the skin
Strictures/Stenosis
Strictures are narrowing of tubes resulting in stenosis and obstruction.
In a study by Parikh and colleagues, stenosis had an incidence rate of 3.5%.6
Common symptoms
- Difficulty in swallowing
- Nausea/vomiting
- Inability to transition to solids from liquids
- Food stuck in esophagus (impaction)
- Food regurgitation
Contrast swallow test or endoscope may be used to assess possible strictures.
Treatment
- Dilation therapy (using endoscope)
- Stenting
- Gastric sleeve revision to Roux-en-Y bypass (as a last resort)
Nutritional Deficiencies
After sleeve surgery, the stomach’s acid production gets inhibited. These stomach acids play a vital role in breaking down protein and converting minerals into absorbable form. This may result in nutritional deficiencies.
Gastric sleeve restricts the amount of food you eat, thereby limiting the amount of vitamins and minerals your body gets. It can also make you intolerant to certain foods packed with nutrients. Hence, taking nutritional supplements becomes a way of life after gastric sleeve surgery.
Johns Hopkins Medicine recommends:
- 1 or 2 multivitamins daily for the entire life
- 1,500 mg of calcium per day (to be divide into 3 doses of 500-600 mg each)
- 3,000 International Units of Vitamin D3daily
- A dose of 500 mg (every day) or 1,000 mg (every alternate day) of Vitamin B12 tablets (to be kept under the tongue)
Regular blood work is recommended for diagnosing nutritional deficiencies.
Gastroesophageal Reflux Disease (GERD)
 Also known as acid reflux, GERD is a condition in which the stomach’s contents leak back into the esophagus.
Also known as acid reflux, GERD is a condition in which the stomach’s contents leak back into the esophagus.
In a research study by Carter and colleagues, GERD was found in 47% of the patients.7
Common symptoms are:
- Fullness behind the breastbone
- Burning sensation in the chest (heartburn)
- Feeling nauseated after eating
- Regurgitation
Persistent acid reflux can be treated through proton pump inhibitors.
If GERD still persists, diagnosis is made through gastroscopy.
References:
- Alvarenga ES, Lo Menzo E, Szomstein S, Rosenthal RJ. Safety and efficacy of 1020 consecutive laparoscopic sleeve gastrectomies performed as a primary treatment modality for morbid obesity. A single-center experience from the metabolic and bariatric surgical accreditation quality and improvement program. Surg Endosc. 2015 Nov 5. PubMed
- PL-104: National Comparisons of Bariatric Surgery Safety And Efficacy: Findings from the BOLD Database 2007-2010. Dr. John Morton; Bintu Sherif, Deborah Winegar, PhD; Ninh Nguyen MD, FASMBS; Jaime Ponce, MD, FASMBS; Robin Blackstone, MD, FASMBS
- Sarkhosh K, Birch DW, Sharma A. Karmali S. Complications associated with laparoscopic sleeve gastrectomy for morbid obesity: a surgeon’s guide. Can. J. Surg. 2013;56:347–352. [PubMed]
- Abou Rached A, Basile M, El Masri H. Gastric leaks post sleeve gastrectomy: review of its prevention and management. World J Gastroenterol. 2014;20:13904–13910.
- Bekheit M, Katri KM, Nabil W, Sharaan MA, El Kayal ES (2013) Earliest signs and management of leakage after bariatric surgeries: single institute experience. Alexandria J Med 49(1):29–33
- Management options for symptomatic stenosis after laparoscopic vertical sleeve gastrectomy in the morbidly obese. Parikh A, Alley JB, Peterson RM, Harnisch MC, Pfluke JM, Tapper DM, Fenton SJ. Surg Endosc. 2012 Mar; 26(3):738-46.
- Association between gastroesophageal reflux disease and laparoscopic sleeve gastrectomy. Carter PR, LeBlanc KA, Hausmann MG, Kleinpeter KP, deBarros SN, Jones SM. Surg Obes Relat Dis. 2011 Sep-Oct; 7(5):569-72.